ALS eventually causes an inability to speak, eat, move and breathe. Hospice for ALS provides relief and comfort to those in the end stages of this incurable disease.
Amyotrophic Lateral Sclerosis, commonly referred to as ALS, is a progressive neurodegenerative disease. The nerves responsible for voluntary motor movements lose their function and die. As they do, the brain can no longer initiate and control muscle movements like walking and talking.
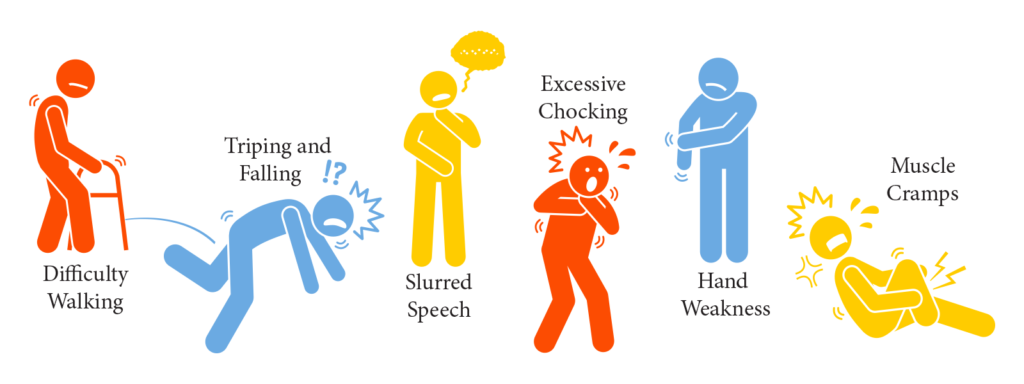
With ALS, the symptoms begin gradually and can vary from person to person, depending on the nerves initially affected. Symptoms often begin with weakness in one limb. As they become more widespread, they can include difficulty walking, tripping, falling, slurred speech, excessive choking, weakness, fatigue, and muscle cramps.
ALS symptoms worsen over time. As more and more nerves are affected, more and more functions become impaired. Eventually, all cases result in near total paralysis and an inability to speak, eat, move, and even breathe. Patients with ALS rely 100% on others for help with normal daily activities.
ALS Symptoms
Recognizing ALS symptoms as soon as possible is essential because it will allow you to get treated sooner. Because ALS has a gradual onset, it will enable you to get tested and determine if you have the disease. As mentioned, symptoms will often begin in one limb, and the initial symptoms can vary from person to person. For example, a patient may notice that they struggle to grab a pen or lift a glass to their mouth, while another patient may experience a change in their voice.
Symptoms vary as the disease progresses, as well. The progression rate differs per patient, with some patients living up to five years with the disease while others live up to 10 additional years. While not all ALS patients experience the same symptoms or even sequences or patterns of progression, nearly all patients experience increasing muscle weakness and paralysis. Some of the most common ALS symptoms include:
Hand weakness
As one of the first-noticed ALS symptoms, identifying hand weakness is one of the first ways that many doctors will diagnose the disease. Because ALS causes weakness and wasting of two hand muscles, doctors will perform a pincer test, also known as a split-hand index, to help identify patients who have the disease.
Muscle twitches
Muscle twitches are one of the most common ALS symptoms, affecting motor neurons. ALS damages worsens, and even kills these motor neurons.
Muscle weakness
In the same way that ALS affects the motor neurons to cause muscle twitches, the same neurons also cause muscle weakness. Muscle weakness can lead to other issues within the body, such as difficulty chewing, eating, and swallowing. Eventually, patients may experience choking.
Muscle stiffness
Many patients report that muscle stiffness is one of the first symptoms of ALS. Muscle stiffness can affect a single body region or even more than one. It can also cause muscle wasting or cramps.
Slurred and nasal speech
Slurred or nasal speech is one of the most recognizable symptoms of ALS. What begins as slurred words often progresses to the point where the speech is almost impossible to understand. Patients lose articulation and begin to speak more slowly with nasal tones and a hoarse, nasally-sounding voice.
Tripping and falling
Because of the disease’s ability to affect muscle and nerve function, patients may experience tripping and falling. Fatigue and poor balance are other common symptoms of ALS that can trigger tripping or falling.
Behavioral changes
Unfortunately, some patients also experience behavioral changes as they progress through the disease. Some common behavioral changes are inappropriate behavior, loss of social skills, decreased attention to hygiene, loss of judgment, inability to concentrate, and increased aggression.
How do I Treat ALS?
Therapies for ALS target symptom management. Depending on the extent of ALS, these could include treating the following:
- Sialorrhea (excessive salivation or drooling)
- Pain
- Muscle cramps and spasticity
- Cognitive impairment
- Dyspnea (difficulty breathing)
- Fatigue
- Physical, occupational, and speech therapies can help a patient adapt to communication and physical limitations due to ALS.
While some drug treatments have shown benefit in delaying physical decline, there are no treatments to reverse the neural damage. Ultimately, ALS is fatal.
When does a Person with ALS Qualify for Hospice?
The first factor that establishes hospice eligibility is the ability to breathe. A patient must show critical impairment in their breathing by having a vital capacity (max volume that can be exhaled) of less than 30% predicted or by experiencing dyspnea at rest.
A patient also may qualify for hospice if they have a rapid progression of the disease. This is demonstrated by any of the following changes over a 12-month period:
- Progression from walking to wheelchair to bed bound
- Normal speech to barely intelligible speech
- Normal to pureed diet
- Independence to reliance for activities of daily living
This rapid progression, along with either a critical nutritional impairment or other life-threatening complications would make a person eligible for hospice.
Managing ALS with Active Hospice
Remember, hospice is not a bad thing. It is not giving up nor does it speed up the dying process. Hospice takes the focus away from the disease process and puts the focus back on you as a person.
The best news is that good ALS treatment is what hospice is best at. ALS treatment is symptom based and that doesn’t change with hospice. We will continue to provide the best possible treatment of all your symptoms. On top of that, our team will address your emotional, spiritual, and social needs as well.
Some of the benefits from managing your ALS with Active Hospice include:
- Continued symptom management
- Improved pain control
- Improved hydration and nutrition
- Better end of life planning
- Assistance with everyday tasks
- Prevention of bed sores
- Emotional support for you and your family
- Bereavement services for loved ones
- Care from the comfort of your home
Why Choose Active Hospice?
Active Hospice’s goal is to help you and your loved ones get the sense of closure that everyone wants at the end of life. We focus on avoiding a prolonged dying experience. This allows us to give you the chance to have an improved quality of life, better control over those end of life decisions, and improved comfort care. Our end of life care plans create opportunities for lasting memories and more enjoyable moments. If you or a loved one are struggling with ALS, give Active Hospice a call and schedule your free, in-home consultation today.