Life is never the same for those who survive sepsis. Learn how hospice helps deal with post-sepsis complications towards the end of life.
Sepsis is the body’s extreme response to an infection. It is a life-threatening medical emergency. Sepsis occurs when an infection that you already have triggers a chain reaction throughout the body. These infections can originate in the lungs, urinary tract, skin and elsewhere. Without timely treatment, sepsis rapidly leads to tissue damage, organ failure, and even death.
Anyone can get an infection and almost any infection can lead to sepsis. Like most diseases, there are certain risk factors that can make you more susceptible to developing sepsis. These include:
- Age over the age of 65
- Chronic and serious illness including cancer, diabetes, COPD, CHF, obesity and chronic kidney disease.
- Impaired immune system
- Trauma and burns
- Previous survival from sepsis
When an infection does lead to sepsis, it usually does so very rapidly. Sepsis most commonly presents with symptoms of fever, chills, and an increase in both heart rate and respiratory rate. If not treated, symptoms worsen and become more serious. Confusion, nausea, vomiting, and disorientation give way to inadequate blood flow and shock as affected organs begin to shut down.
Treatment for sepsis is given in the hospital, usually in the ICU. A patient is given an antibiotic to treat the infection. They are also given fluids to help prevent organ damage and to sustain blood pressure. Each year, 1.7 million American adults develop sepsis. 1.4 million survive.
Complications from Sepsis
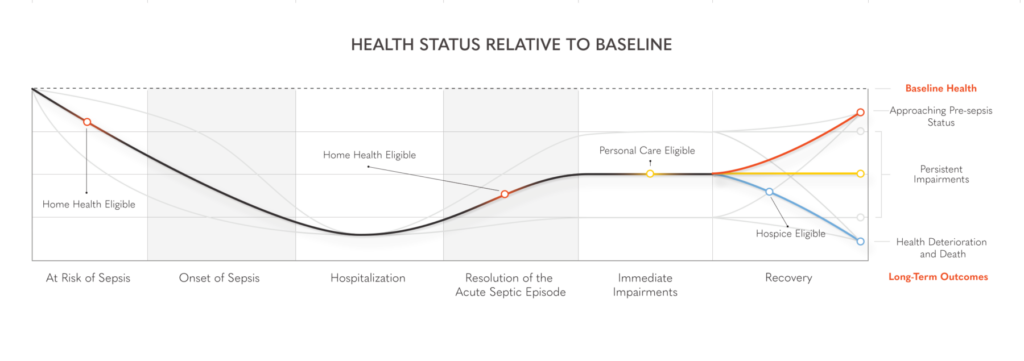
Unfortunately, studies have shown that life is never the same for those 1.4 million adults. On average, only half of those adults will fully recover. A third die within the following year and a sixth of those patients will have some sort of functional impairment stemming from sepsis.
Patients that survive sepsis often develop new symptoms. One of the most common set of symptoms involve changes in their cognition and mental health. Sepsis patients report higher levels of anxiety, depression, and PTSD. They often have long-term impairments to their memory and attention. They are at an increased risk of reinfection, trouble sleeping, and have reported higher levels of pain.
Patients who survive sepsis also develop long term disabilities. On average, they report having to adapt or change 1 to 2 normal daily activities. They often have trouble swallowing and report higher levels of aspiration. While they may regain some physical strength after discharge, they usually do not return to their pre-sepsis level of activity. Many cannot resume prior roles and activities.
On top of everything else, sepsis has been shown to potentially worsen a patient’s other chronic health conditions. Patients who survive typically experience higher levels of hospitalizations for exacerbations of heart failure, renal failure, and COPD. They also experience a greater number of cardiovascular events, like heart attacks, than the normal population.
As stated above, individuals who survive sepsis are still at an increased risk of dying, especially within the first year. Some factors that are associated with an increased risk of dying in the first year include age greater than 85, presence of other comorbid diseases, like CHF or COPD, dependency in multiple ADLs, 2+ hospitalizations in the past 12 months, living in an assisted living setting or an overall poor health status.
Managing Sepsis Complications with Active Hospice
Like any major, chronic condition, preparing for that final journey can be a stressful event. Active Hospice is here to help. Remember, hospice does not mean giving up nor does it speed up the dying process. Hospice takes the focus away from the disease process and puts the focus back on you as a person. At Active Hospice, we believe in offering you control, quality and comfort during life’s final journey.
Some of the benefits of using Active Hospice to help with post-sepsis symptoms and decline include:
- Improved management of long-term symptoms,
- Better pain control
- Better support of the patient and family
- Improved spiritual well-being
- Better end of life planning
- Prevent rehospitalization
- Improved quality of life
- Decreased number of invasive procedures
Why Choose Active Hospice?
Sepsis is a life-threatening emergency that, even when survived, alters lives. Most patients develop complications and experience a decrease in life expectancy. Active Hospice is here to serve you through life’s final journey. Our end of life care plans are designed around your needs. Our care team helps you and your loved ones attain a sense of closure and understanding that allows you to experience the quality, control and comfort up to the end. Give us a call today to schedule your free, in-home consultation.